The genuine healthcare predicament in India lies in the specter of financial burden
In the intricate world of healthcare, the cost of quality care is a topic of ongoing debate. The Indian healthcare landscape is particularly complex, with a myriad of factors influencing pricing.
The cost of healthcare includes a complex ecosystem that must remain active and prepared at all times. This includes clinical staffing, emergency readiness, critical care infrastructure, infection control systems, and adherence to quality and safety standards. Advances in healthcare such as precision oncology, robotic surgery, and AI-supported diagnostics require significant investment but offer improved outcomes, reduced complications, and shorter hospital stays.
However, variations in healthcare pricing in India are influenced by multiple factors. Geographical Location plays a significant role, with urban areas like Delhi, Mumbai, and Bangalore having higher healthcare costs compared to rural regions due to better infrastructure, availability of advanced medical facilities, and higher cost of living.
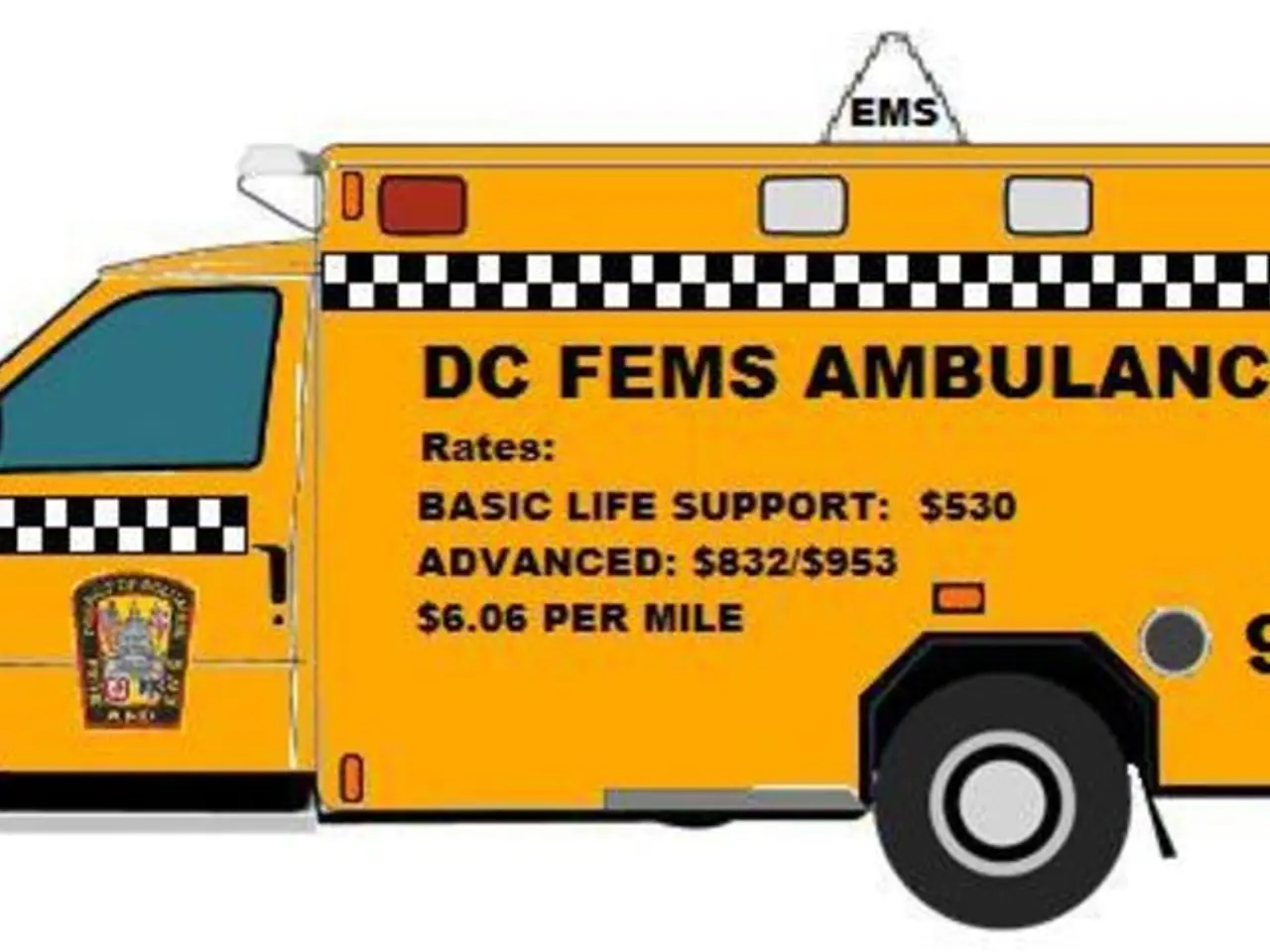
Healthcare costs rise faster than general inflation, primarily due to expensive hospitalisation, diagnostics, medicines, and adoption of advanced medical technologies that enhance care quality but increase costs. Age, health profile, sum insured, coverage type, and policy duration play crucial roles in determining insurance premiums, indirectly affecting healthcare affordability and access.
India has a high share of out-of-pocket payments (about 48% of total healthcare spending), which is a major affordability barrier. This financial burden often forces low-income households to forgo or delay care, negatively impacting outcomes and quality.
These components are not optional extras but integral components of quality care. Well-structured health insurance plays a vital role in shielding individuals and families from the financial impact of medical treatment. Seeking healthcare should not be seen as a luxury but as a fundamental investment in quality of life, productivity, and the ability to care for others.
Moreover, hospitals are increasingly investing in digital tools and proactive counselling to support this process. Over 2.5 million individuals screened by Apollo Hospitals in the past year revealed that nearly one in four were living with diabetes or hypertension, often undiagnosed.
The data from the screenings also highlighted a sharp rise in obesity and pre-hypertension among younger adults. More than 65% of the individuals screened had fatty liver disease, frequently without symptoms or known risk factors.
Attempts at price capping in healthcare have historically led to reduced supply, quality decline, or corruption, suggesting that pricing controls alone cannot resolve disparities in care quality. Trust in healthcare can be built when care is accessible, transparent, and humane. Solutions must be rooted in compassion and shaped by the belief that timely care should never be out of reach.
In summary, variations in Indian healthcare pricing reflect complex interactions between economic, geographic, technological, and insurance-related factors, which simultaneously drive improvements in some areas while creating affordability and quality challenges in others. Shifting the mindset in this direction requires more than awareness; it calls for action - broader and simpler insurance coverage, easier access to credible information, and stronger partnerships between providers, policymakers, and communities. The cost of neglect in healthcare can be far greater than the cost of care itself. Clearer, more transparent communication about healthcare pricing can help patients prepare, understand what is included in a package, and ask the right questions.
- Investment in infrastructure like critical care facilities, vaccination centers, and advanced medical technologies is essential for enhancing healthcare coverage.
- The price of healthcare policies often varies based on the type of coverage, policy duration, and individual health profiles.
- Lack of proper investment in infrastructure and technologies can lead to poor coverage and inadequate care.
- Despite advances in Science, chronic diseases like cancer, respiratory conditions, and digestive health issues continue to pose significant challenges.
- Workplace-wellness programs can help manage medical conditions related to diabetes, hypertension, and obesity, promoting fitness-and-exercise and nutrition.
- Annual medical checkups and regular screenings can help early detection and management of eye-health, hearing, and skin-conditions.
- Autoimmune disorders, mental-health issues, and men's-health concerns are often overlooked yet require immediate attention and appropriate therapies-and-treatments.
- Robust policies should consider the needs of women, addressing concerns related to womens-health, skin-care, and reproductive health.
- Pregnancy, childbirth, and parenting also require proper medical attention and support, affecting both physical and mental health-and-wellness.
- Skin-conditions and neurological disorders can significantly impact a person's quality of life, requiring appropriate treatments and management.
- Personal-finance management, wealth-management, and education-and-self-development are essential for minimizing healthcare costs and preventing financial crises.
- Career development opportunities in healthcare help attract skilled professionals, ensuring better care and improved outcomes.
- Weight-management and cardiovascular-health are critical areas of concern, requiring proactive measures and lifestyle changes for prevention.
- Medicare and insurance providers should ensure affordable and comprehensive coverage for all, prioritizing the needs of elderly individuals and those with low incomes.
- Policymakers must work towards strengthening the healthcare system, focusing on financial assistance, facility upgrades, and employee training to enhance care quality.
- Advocating for increased public funding, tax incentives, and partnerships between public and private sectors can help reduce the burden of healthcare costs.
- Transparency in pricing can lead to improved patient satisfaction, trust, and better decision-making when choosing health-and-wellness services and treatments.
- Aging gracefully should not be limited by the availability or cost of medical care, with the focus on maintaining overall wellness and preventing age-related conditions.
- Better access to mental-health resources and support can help manage stress, anxiety, and depression, contributing to overall mental and emotional well-being.